IFT in Ventral Hernias
Evangelisches Krankenhaus Herne, Germany - April 2025
Emile Rijcken successfully carried out a surgery on a 32-year-old patient (BMI: 24.5, ASA II), in which a ventral hernia was caused by an open abdomen due to biliary necrotising pancreatitis and impossible fascial closure. Therefore, it was left to heal over an abdominal apertum, and the wound was covered with a skin graft, which was placed directly on the adhered bowel. Because of the biliary pancreatitis and the stone-filled gallbladder that was still in situ, a simultaneous cholecystectomy was performed. The removal of the skin graft posed a particular challenge in this case.

Clinical examination
Clinically, there was a pronounced abdominal wall defect due to the previous patient history as described above.

CT Scan
The CT scan showed a 16 x 18 cm ventral hernia with no significant loss of domain. The small intestine was directly adjacent to the skin graft, suggesting that extensive adhesiolysis and preparation would be required.
Pre-treatment with Botulinum Toxin A
Prior to surgery, the patient was pretreated with Botulinum Toxin A to achieve maximum relaxation of the lateral abdominal wall.
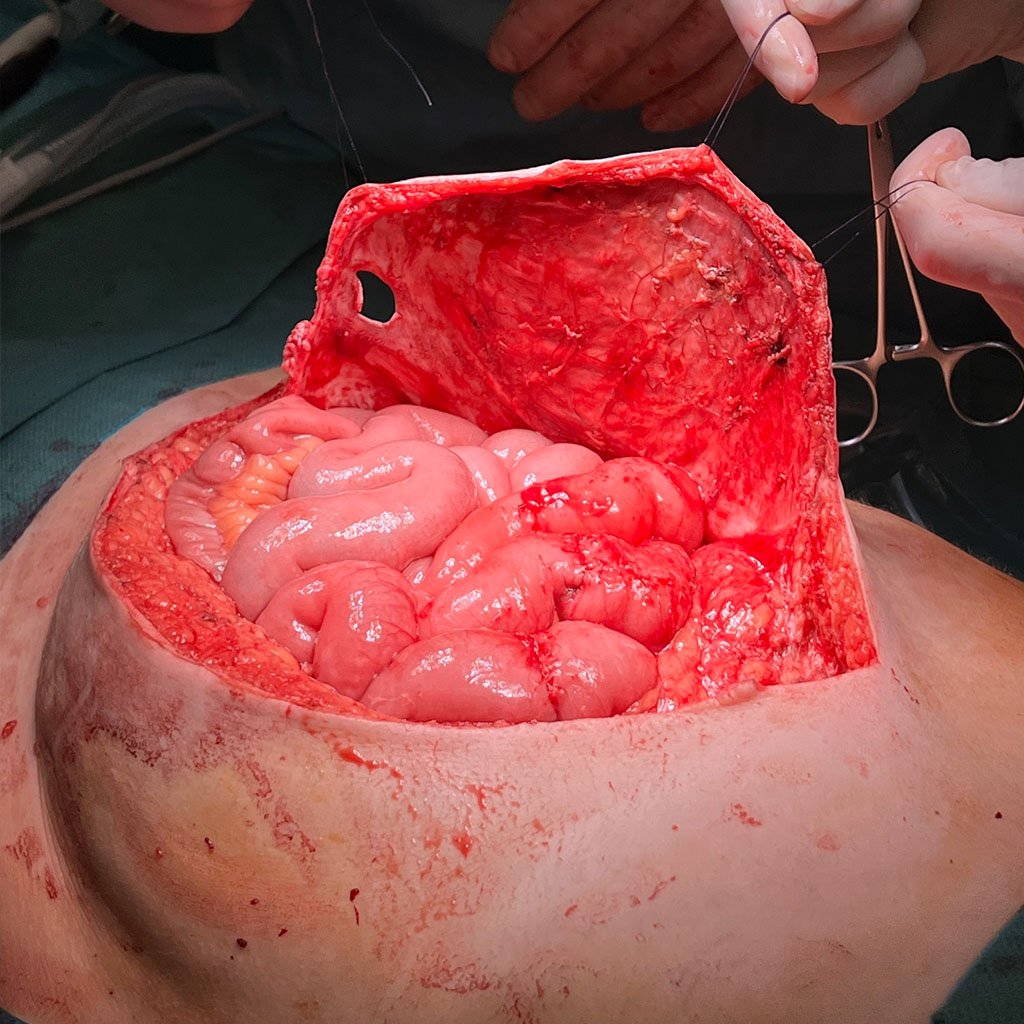
Removal of the skin graft
During surgery, the skin graft was carefully detached first. A cholecystectomy was performed before treatment of the hernia was started.

Rives-Stoppa Preparation + Flap
The rectus sheath was opened on the right side ventral to the flap and the posterior rectus sheath was dissected far lateral to the transverse muscle while preserving the perforating vessels and the epigastric vessels. The procedure war repeated on the left side, incising the rectus sheath on the dorsal side of the flap. The dissection was performed cranially up to the xiphoid process and costal arch, and caudally down to the symphysis.
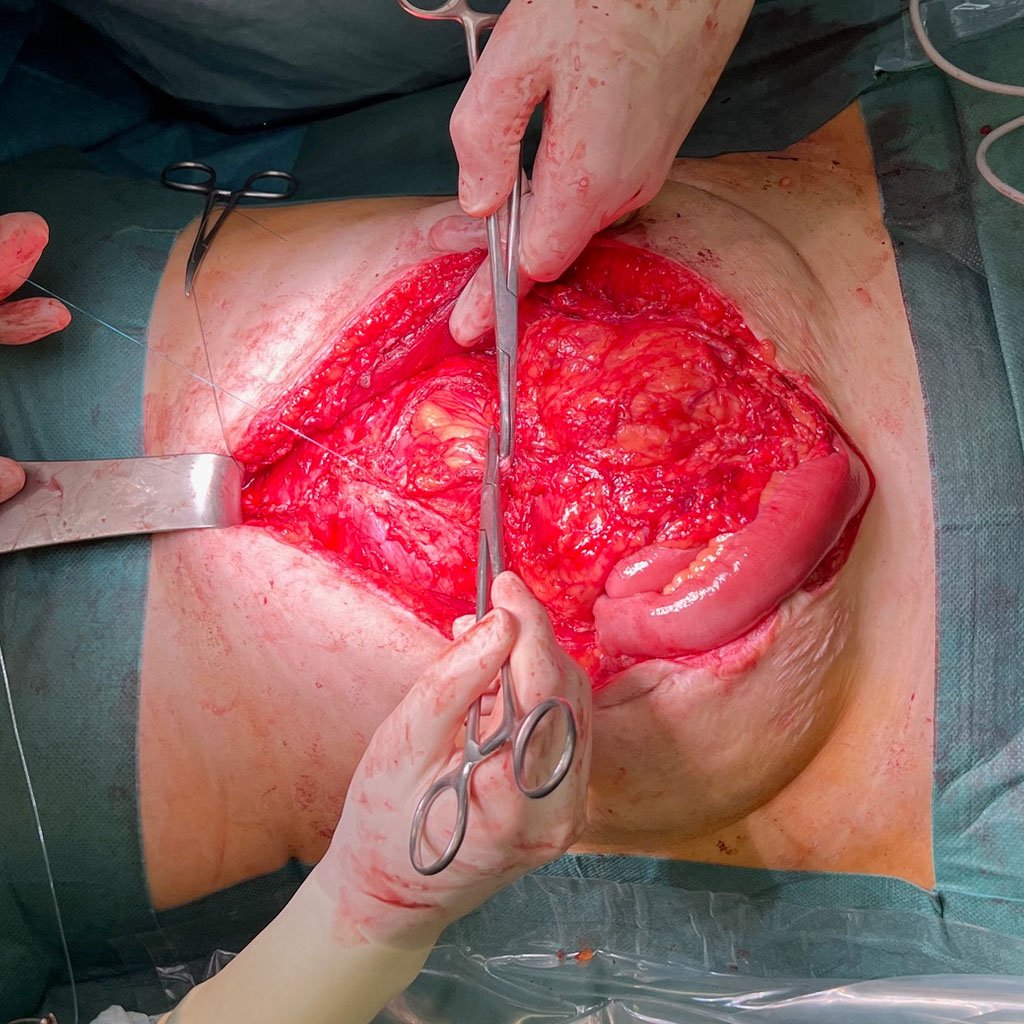
Closure of the posterior rectus sheath
Thanks to Botulinum Toxin A, the two posterior layers could already be approximated. After appropriate mobilization, the omentum was placed over the complete bowel. The posterior layer was closed with a continuous 2-0 Maxon suture.

Sublay-Mesh
A Dynamesh CICAT was trimmed to dimensions of 13 cm × 30 cm with rounded corners. The mesh was positioned on the closed posterior rectus sheath without tension or folds and secured using 2-0 Surgipro sutures in a U-stitch configuration. A closure of the anterior fascia was deemed impossible, so intraoperative fascial traction was performed.

Intraoperative fascial traction (IFT)
On each side of the defect, 6 USP 2 vicryl sutures were inserted using a U-stich technique. The crossed sutures were fixed into the suture retention frame of the fasciotens®Hernia device. IFT was performed for 30 minutes with a traction force of approx. 16-18 kg. During traction, the ventilation pressure remained stable at 14 mmHg, with no increase due to closure of the abdomen.
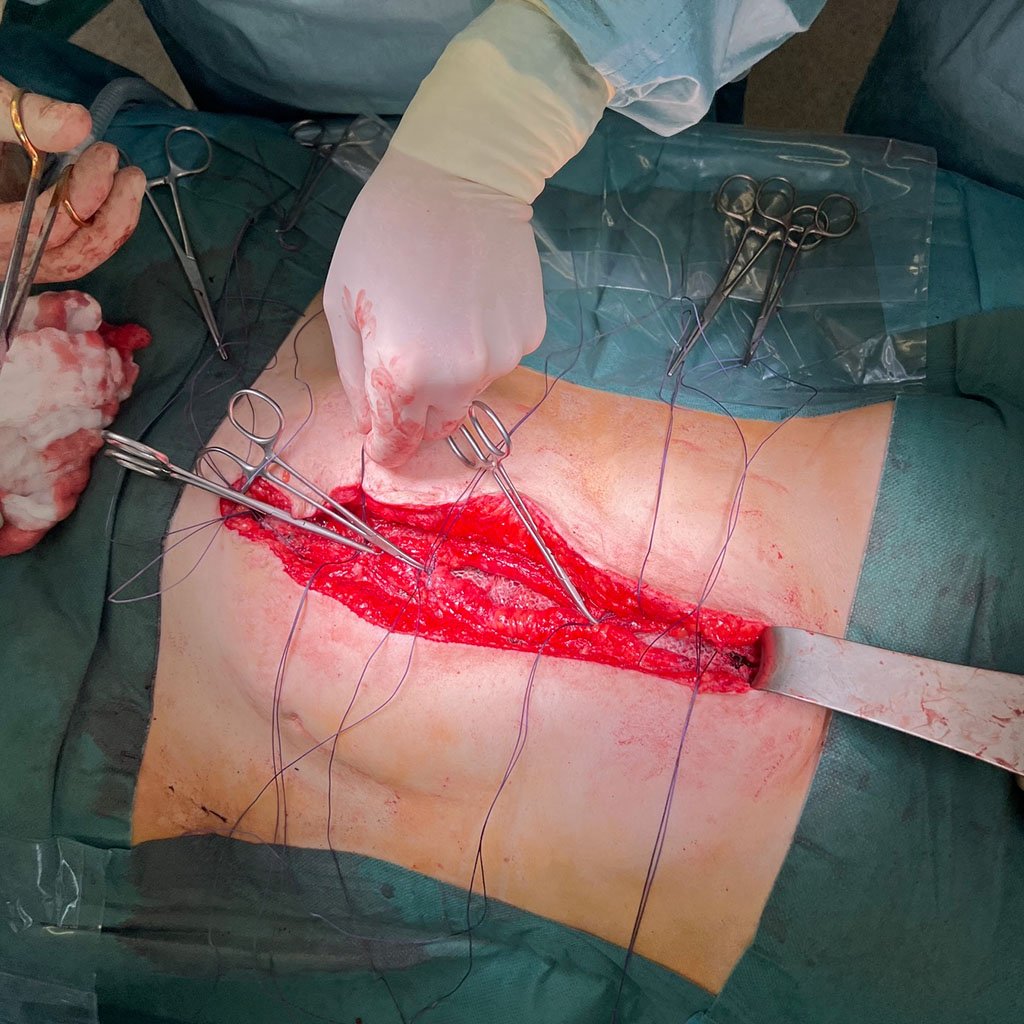
Clousure of the anterior rectus sheath
The anterior fascia was successfully closed using the small-bites technique with a 2-0 Maxon suture.

Result before skin closure

Result after skin closure

Postoperative cosmetic result
Postoperative result on the 19th day after surgery.

Prof. Dr. med. Emile Rijcken
Specialist in general and visceral surgery, additional qualification in special visceral surgery and proctology

EVK Herne
Germany

Prof. Dr. med. Chris Braumann
Specialist in general and visceral surgery, additional qualification in special visceral surgery and proctology

EVK Herne
Germany
Start with fasciotens yourself
