
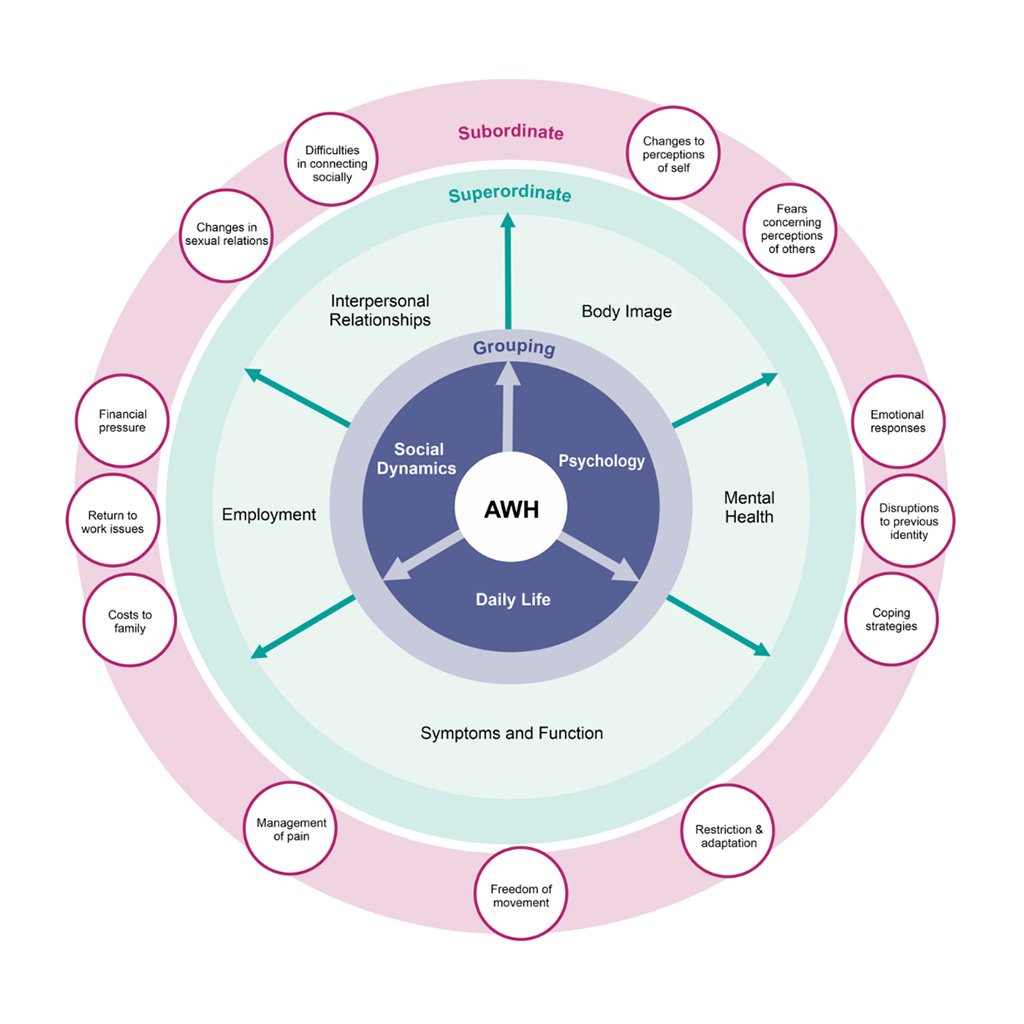
Holistic approach in managing complex abdominal wall hernias
When the case demands the full skill set of AWR surgery
York Abdominal Wall Unit, UK - September 2024
Srinivas Chintapatla (Consultant Colorectal Surgeon) and Tom Macleod (Consultant Plastic Surgeon) at York Abdominal Wall Unit together performed an Abdominal Wall Reconstruction using various techniques, including fasciotens®. Asim Abbas (Abdominal Wall Research Fellow) kindly provided the following case description.
Preoperative Remarks
- The Patient
- Surgical History
- Quality of Life
- Prehabilitation
- BTA
- PPP
Case presentation
This 62-year-old patient presented with a complex, massive recurrent, incisional hernia significantly impacting his quality of life.
The hernia footprint was extensive including a large left-sided hernia (30x30 cm), and additional paraumbilical and midline hernia.
The defects spanned M2, M3, M4, and L regions, and the case was VHWG Grade 2.

Extensive hernia surgery history
2015 - primary right inguinal hernia repair with mesh.
2016 - epigastric and paraumbilical hernia repairs with sublay mesh
2019 - exploratory laparotomy and small bowel resection for an incarcerated recurrent right inguinal hernia.
2019 - redo Lichtenstein mesh repair for a recurrent inguinal hernia.

Severe impact on quality of life
York Abdominal Wall Unit looks into five domains:
- Body image - he described feeling unsightly and uncomfortable, avoiding activities like swimming.
- Mental health was affected, with him being on medication for depression and mentioning that his condition contributed to his divorce.
- Symptoms & Function - he experienced discomfort and avoided physical work.
- Employment - he reported a lack of confidence in seeking employment.
- Interpersonal relationships, particularly his sexual relationship with his wife, were negatively impacted.
Increasing Fitness level
The patient weighed 124 kg, height was 1.75 m with BMI of 40.7, with CeDAR calculation of 66%.
He was enrolled in a prehabilitation program to optimize fitness for surgery.
York runs an 8-week 'prehab' programme to bring about behavioural changes like reduced portion sizes, daily walking, and strength exercises using 3kg dumbbells.
The leaflet on display was handed out to the patient.
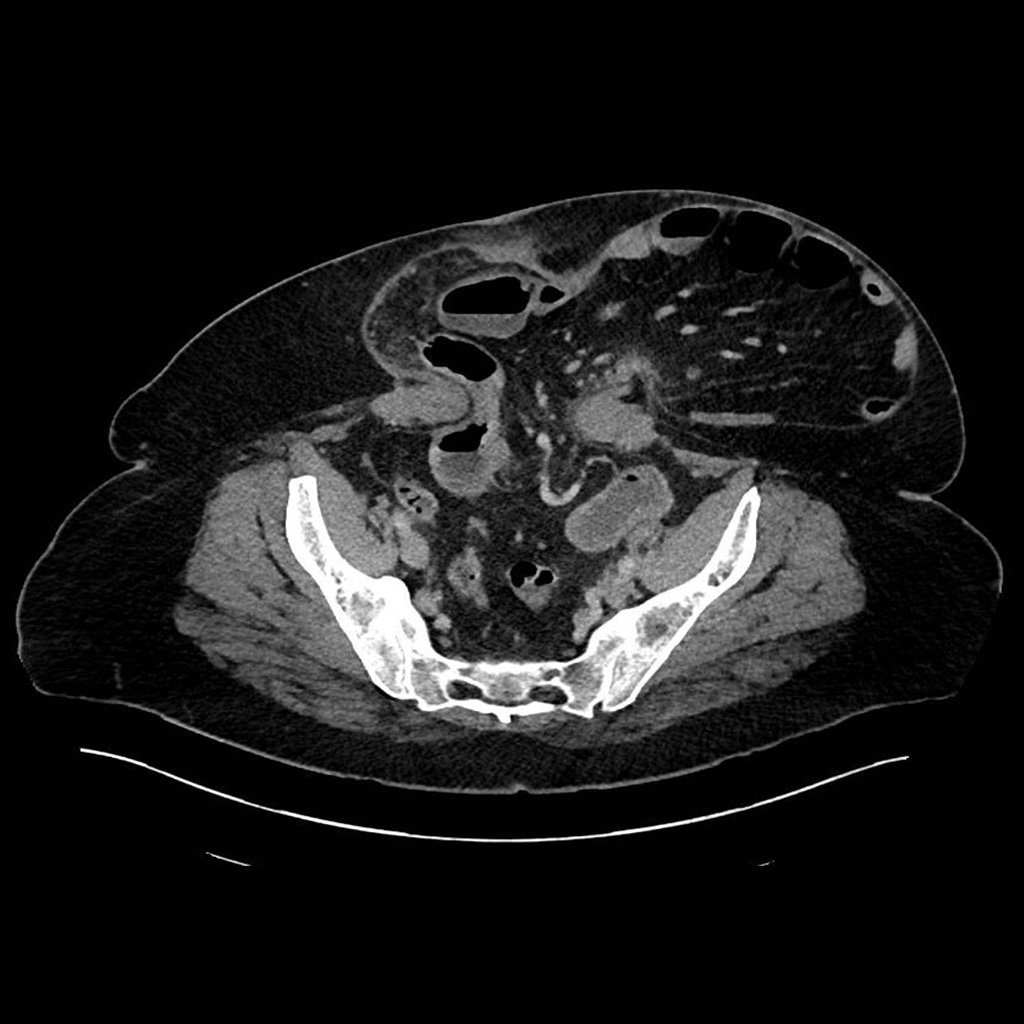
Preconditioning with BTA
During the prehabilitation phase, the patient had an episode of bowel obstruction.
A CT scan at this stage showed significant protrusion and abdominal wall dysfunction.
Botulinum toxin A (Dysport) injections were administered to the abdominal wall, and the obstruction subsequently resolved, although it remains unclear whether the resolution was directly related to the injections.
Continued Preoperative Optimisation
Preoperative optimisation continued with the placement of an IVC filter to manage thrombotic risk. York Abdominal Wall Unit's Progressive Pneumo Peritoneum (PPP) protocol was delivered to increase intra-abdominal volume and improve the feasibility of hernia closure.

Intraoperative Course
- Rives-Stoppa
- Anatomical Reconstruction
- Intraoperative Fascial Traction

Extended Rives-Stoppa Repair
The surgical team performed an extended Rives-Stoppa repair. The retrorectus space was reinforced with Phasix mesh, chosen for long-term durability and resistance to infection. The mesh was carefully tailored to cover the extensive defect.
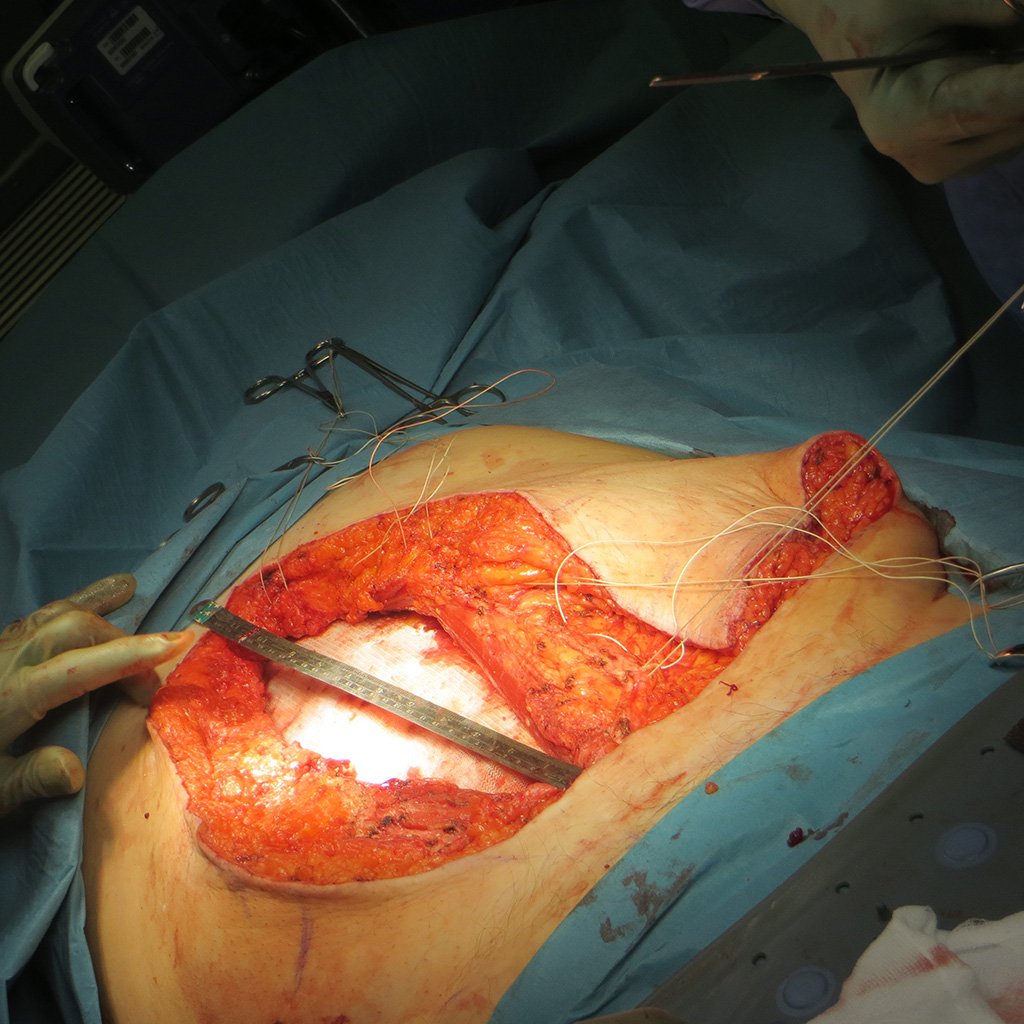
Considerations for IFT
During closure, attention was given to achieving tension-free midline approximation. However, to minimize dissection and reduce the risk of complications, they opted to utilise the fasciotens® device. This allowed the anterior rectus sheath to be mobilised effectively without performing a Component Separation.
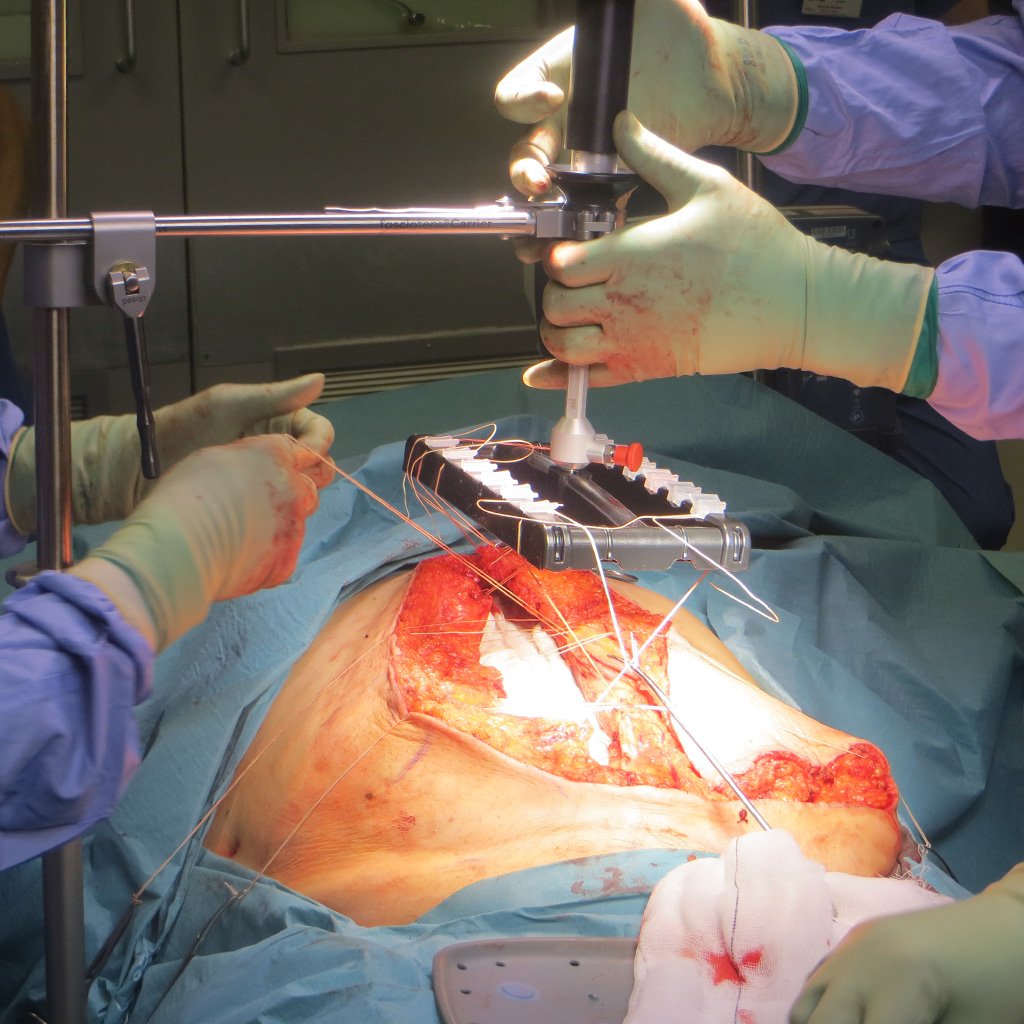
Controlled Traction during IFT
The fasciotens® device was applied to exert controlled tension at 14-18 Kg, gradually bringing the anterior rectus sheath together over 30 minutes.
Postoperative Outcomes
- Postoperative Course
- Quality of Life
- Summary
Discharge on Day 5
Postoperatively, the patient had a good recovery and was discharged on day five. A clinical photo taken three weeks after surgery shows a well-healed abdomen with significant improvement in contour.

Improved Daily Life
The patient reported improvements in quality of life across all domains during follow-up. For:
- Body image - stating, "Now I feel great; my body is in better shape than it has been for years."
- Mental health improved significantly, with him expressing newfound confidence and a sense of rejuvenation.
- Symptoms improved, being able to lift and carry light loads and engage in activities such as gardening, badminton, and swimming.
- Employment - he also regained confidence in seeking employment.
- Interpersonal relationships had greatly improved, particularly with his wife and children. His relationship with his wife had resumed intimacy, which he described as a major positive change.
Satisfying Outcomes
This case highlights the effectiveness of the fasciotens® device in facilitating midline closure in complex hernia repairs with significant loss of domain. The device allowed for tension-free closure, thus sparing component separation, leading to a successful surgical outcome and a marked improvement in the patient’s quality of life. The case also emphasizes the importance of a holistic approach, including prehabilitation and comprehensive quality-of-life assessment, in managing complex abdominal wall hernias.
Read more about York's abdominal wall reconstruction service here.
Srinivas Chintapatla summarises the impressive outcome
The leading surgeon, Srinivas Chintapatla, is very satisfied with the results. The patient is back to a normal life despite the complex history before the abdominall wall reconstruction involving intraoperative fasciotens® application.
The surgeons

Srinivas Chintapatla
Consultant Surgeon – York and Scarborough Teaching Hospital

Tom Macleod
Consultant Plastic, Reconstructive and Cosmetic Surgeon – York and Scarborough Teaching Hospital
Start with fasciotens yourself
