IFT and TAR
Large Incisional Hernia Repair Using Bilateral TAR and IFT
Bürgerhospital Frankfurt am Main, Germany - December 2024
Dr. Terence Alapatt reports this case involving a 61-year-old male (BMI: 34.08) presenting with a large incisional hernia following previous abdominal surgery. Due to the size of the defect and associated loss of domain, a bilateral transversus abdominis release (TAR) combined with intraoperative fascial traction was planned to enable primary closure.
Case Overview
- Patient History
- Preoperative Notes
- Surgical Procedure
- Postoperative Course
A 61-year-old male patient with an initial BMI of 41.28 (reduced to 34.08 after a 23 kg weight loss) presented with a large incisional hernia following emergency surgery in Egypt in December 2022. The initial procedure included a midline laparotomy and a protective colostomy due to perforated sigmoid diverticulitis. In April 2023, the colostomy was reversed.
Preoperative CT imaging (performed one year prior to surgery) revealed a defect size of 23 × 23 cm and a loss of domain of 28% (EHS-Classification: M2-4W3). After botulinum toxin injections (200 IU/90 ml bilaterally into the lateral abdominal wall muscles at three points per side), the scan demonstrated good lateral abdominal wall relaxation and reduced loss of domain. Additional prehabilitation included smoking cessation, respiratory training, and thrombosis prophylaxis the evening before surgery.
A complete adhesiolysis was performed. Bilateral TAR was carried out prior to traction to allow closure of the posterior rectus sheath. Without tension, defect width in the anterior rectus sheath measured approximately 17 cm. Under tension, this distance was reduced to 8–9 cm.
Traction was performed using the fasciotens®hernia device for 30 minutes after closure of the posterior sheath. The maximum traction force applied intraoperatively was 20 kg. By the end of the traction phase, a fascial closure without tension was achieved.
A 43 × 45 cm mesh was placed in the retromuscular position. The anterior sheath was closed directly, without bridging or the need for peritoneal flaps.
No intraoperative complications occurred.
On postoperative day 1, the patient was mobilized and respiratory training resumed. On day 2, the patient experienced dyspnea with an oxygen saturation of 87%. Laboratory results showed an elevated white blood cell count (12.9) and CRP (159 mg/l). A CT scan indicated subtotal atelectasis of the left lower lobe. Bronchoscopy revealed a mucus plug in the left bronchus, which was successfully removed. Cultures were sterile. Antibiotic therapy was administered from day 2 to day 5.
A localized area of reduced perfusion on the lower left abdominal skin was treated conservatively. The patient was discharged on postoperative day 6. On day 14, sutures were removed. The wound continued to heal well, with most of the initially ischemic area showing recovery.
Surgical Steps
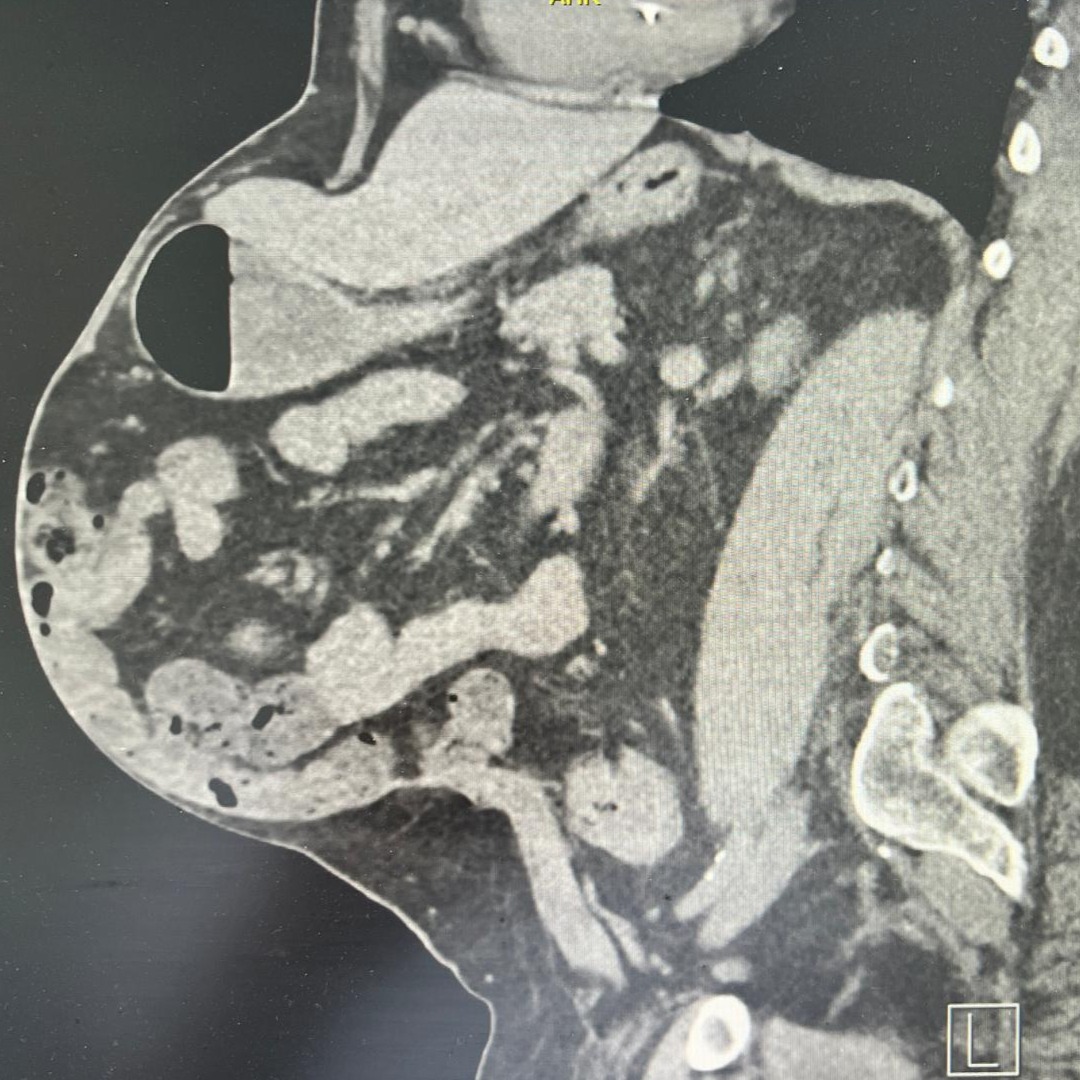
Pre-Operative CT Scan
Large ventral hernia with a defect size of 23 × 23 cm and loss of domain of 28% (EHS-Classification: M2-4W3)

Closure of Posterior Rectus Sheath
Posterior sheath approximation after bilateral transversus abdominis release. Defect size measured 17 cm without tension
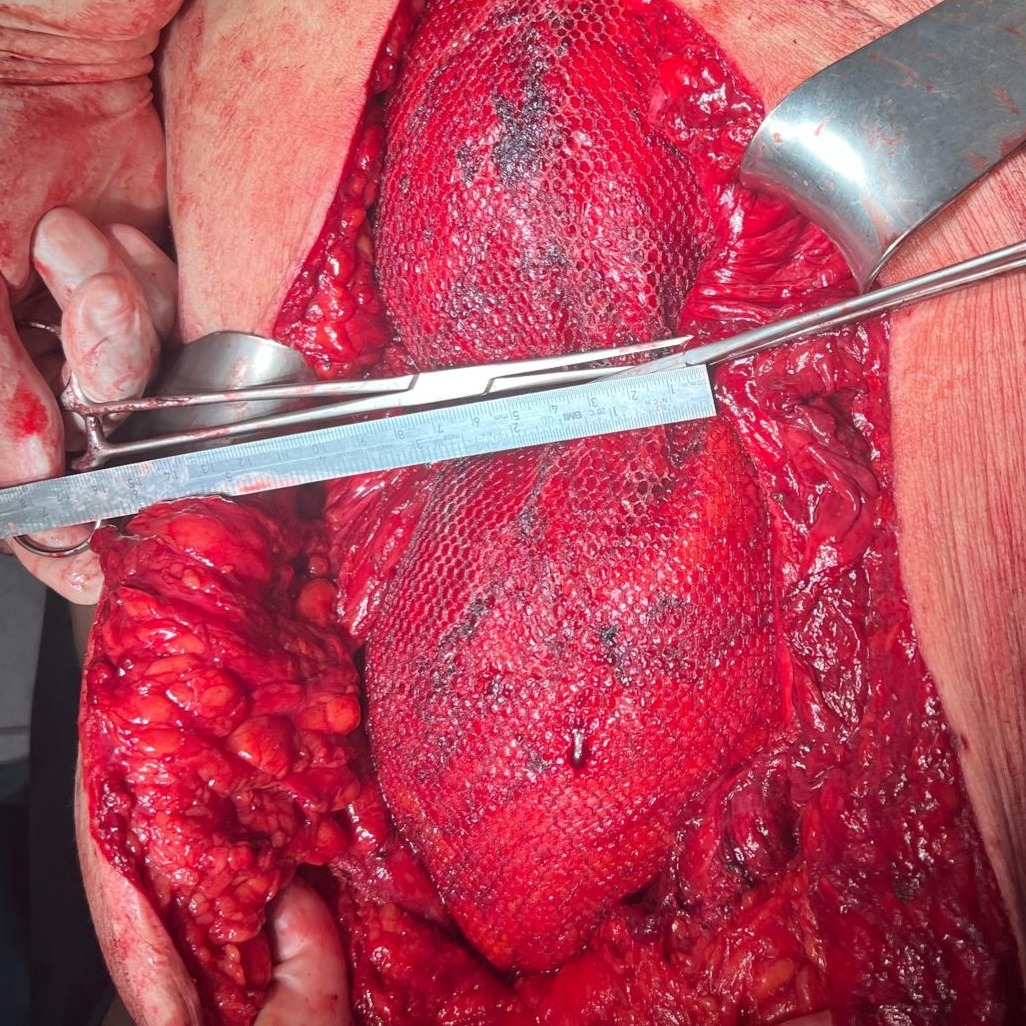
Fascial Defect Measurement
After mesh placement, gap measured at 8–9 cm with manual approximation.
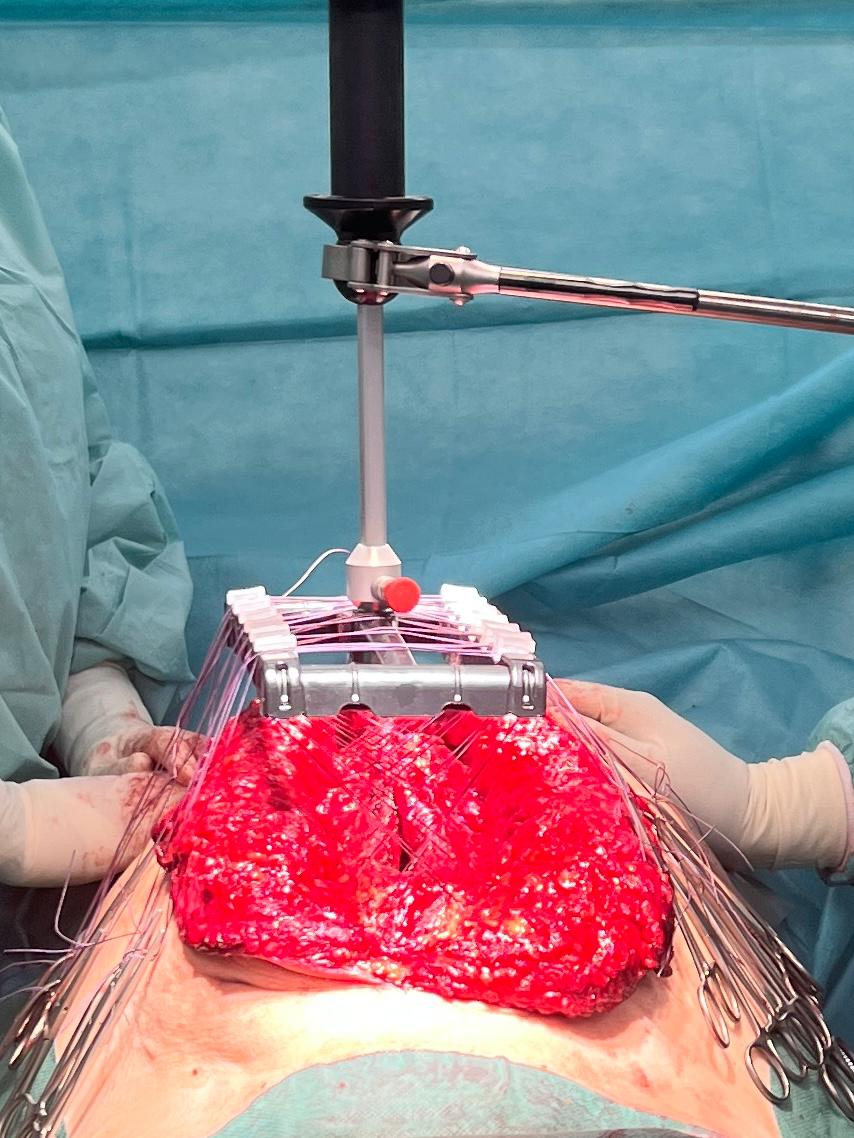
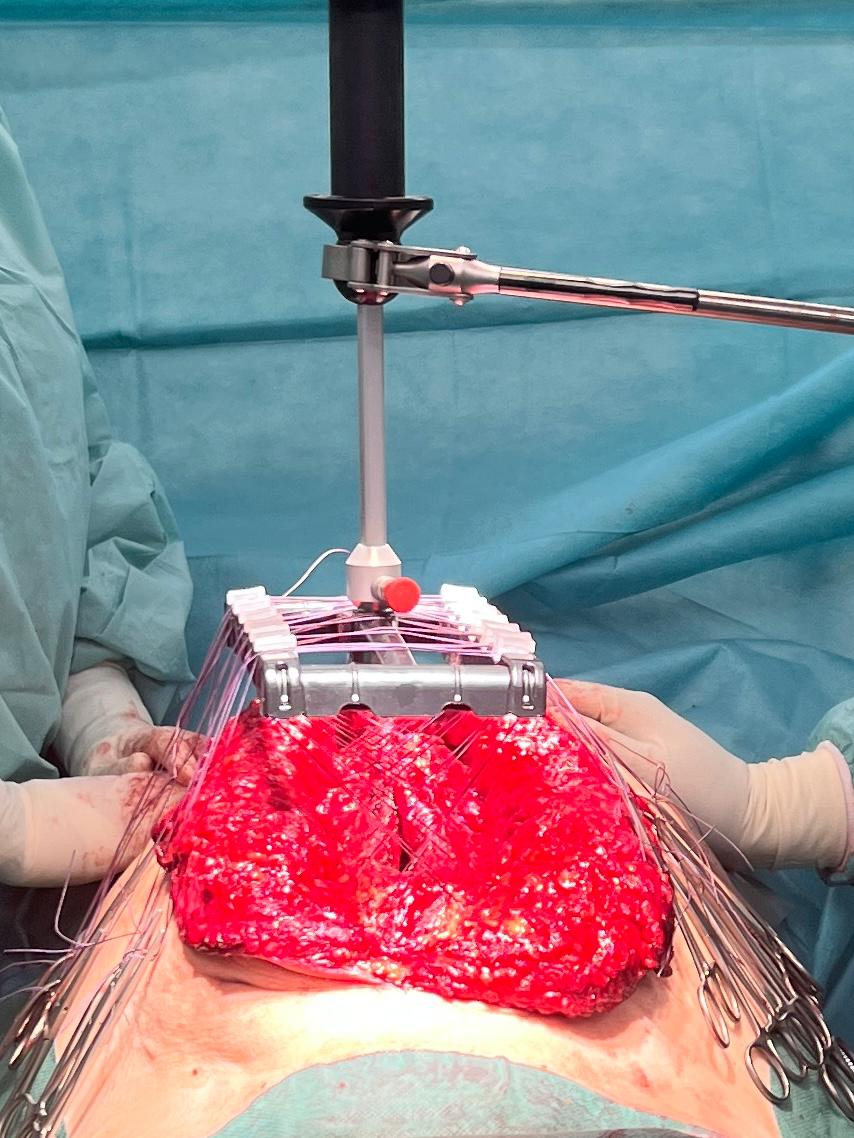
Traction Phase
30 minutes of intraoperative fascial traction applied with forces up to 20 kg.

Completed Anterior Midline Closure
Final midline closure achieved without tension.

Post-Operative Results
Lateral and frontal comparison before surgery and after recovery, showing reduced abdominal protrusion.
Start with fasciotens yourself
